Medical Disclaimer: This guide provides general harm‑reduction information, not medical advice. For personalised care—particularly if you have an ongoing health condition—please consult a clinician experienced in LGBTQ+ health.

Quick Answer: After chemsex, prioritise steady rehydration with electrolytes, easy-to-digest, potassium- and magnesium-rich foods, and small protein-containing meals over 24–48 hours to reduce the severity of the comedown and support recovery.
Introduction
Chemsex can feel intense in the moment, but afterwards, your body needs fluid, electrolytes, and gentle calories to restore balance. Substances like MDMA, methamphetamine, and GHB/GBL commonly cause dehydration, suppressed appetite, and significant electrolyte loss—especially sodium, potassium, and magnesium[5]. Recovery should focus on replacing those losses in a safe and gradual manner.
Key Recovery Priorities
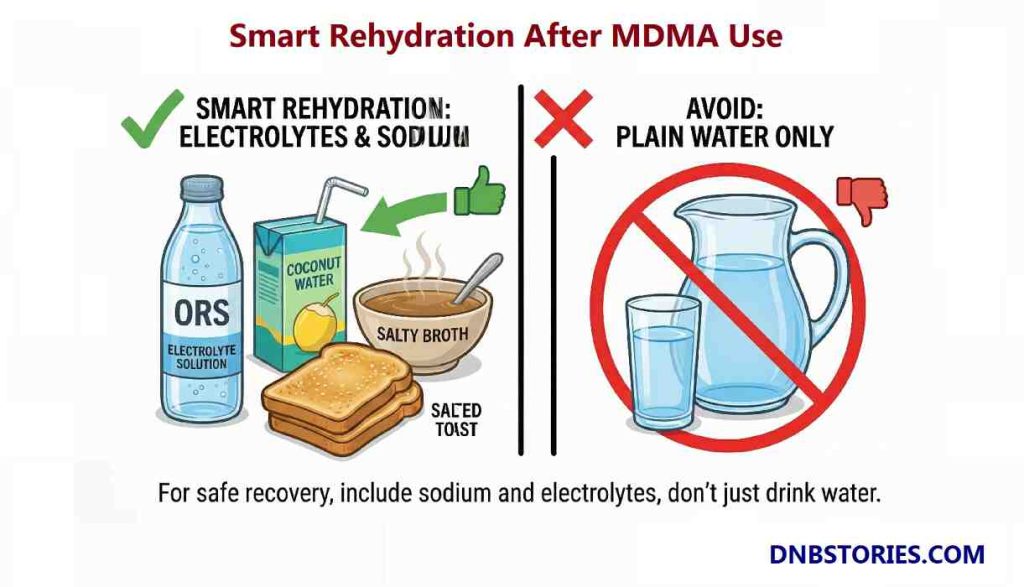
- Hydrate Smart: If MDMA was involved, rehydrate with electrolyte-rich fluids, not just plain water [4].
- Restore Minerals: Replace potassium and magnesium to reduce cramps, fatigue, and mood swings.
- Gentle Fuel: Start with small, frequent, easy-to-digest calories and some protein to stabilise blood sugar and boost cell regeneration.
Important Safety Note: The Water Risk
MDMA poses a specific water risk. If you have used MDMA, drinking excessive amounts of plain water can be dangerous. It can contribute to hyponatremia (critically low blood sodium), a condition that can be fatal (Baggott et al., 2016)[1].
The Rule: If you are thirsty, sip steadily—but you must include electrolytes (salt), not just plain water.
Practical Tip: Take small sips of an oral rehydration solution (ORS) or coconut water plus a salty broth or salted toast rather than only plain water[3].
Sodium Amount/Measurement: A general guideline is to include a moderate amount of sodium during early rehydration—roughly what you’d get from a few servings of a standard electrolyte drink or a mug of salty broth. This helps the body retain fluids and rehydrate effectively without over‑diluting electrolytes.
Top Foods for Chemsex Recovery and Why They Help
| Food | Hydration | Electrolytes | Protein | Ease of Digestion |
| Banana | Moderate | High (Potassium) | Low | Very Easy (Mashable) |
| Watermelon / Melon | Very High | Low–Moderate | None | Very Easy (Cooling) |
| Salty Broth / Soup | High | High (Sodium) | Variable | Very Easy (Warming) |
| Greek Yogurt | Moderate | Low | High | Gentle (Probiotic support) |
| Oatmeal | Low–Mod | Low | Moderate | Soothing, slow carbs |
Practical 48‑Hour Recovery Plan
We have ensured that this is realistic and tested; however, it is not perfect. If you can’t eat, prioritise fluids.
First 6–12 Hours (The Crash Phase)
- Action: Sip an oral rehydration or electrolyte drink slowly.
- Food: Small portions of salty broth and a banana or melon slice.
Day 1 (Stabilise)
- Breakfast: Smoothie (banana + berries + yoghurt + coconut water).
- Snack: Small bowl of warm oatmeal or salty broth.
- Dinner: Lentil or vegetable soup.
Day 2 (Gradual Build-Back)
- Breakfast: Oats with nuts.
- Lunch: Scrambled eggs with spinach (magnesium source).
- Dinner: Salmon or other fatty fish (for omega‑3 support) when appetite returns.
Vegan Alternatives:
- Tofu for protein
- flaxseeds for omega-3s
- Plant-based yogurt (e.g., almond or coconut)

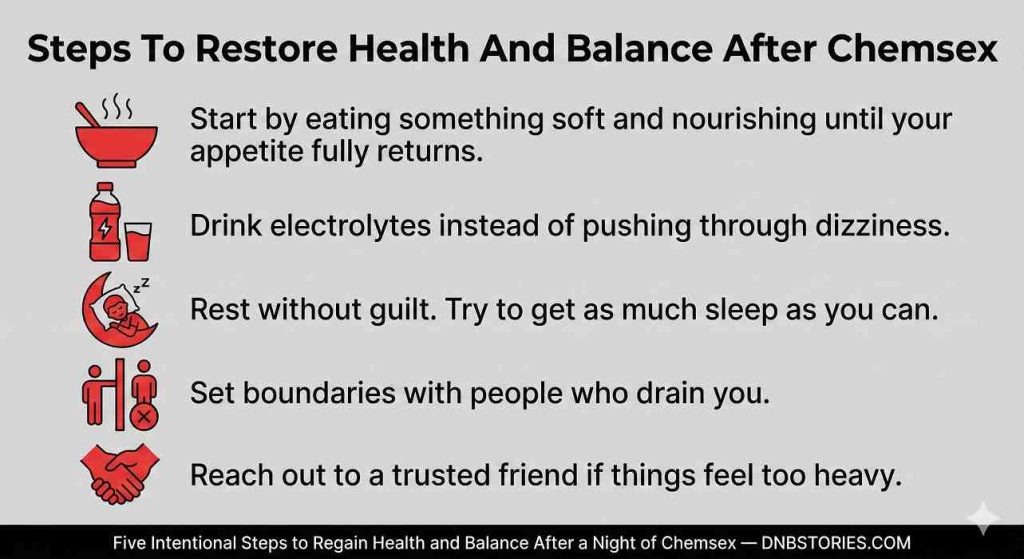
Cultural and Emotional Aftercare
Recovery after chemsex is both physical and social—for Black gay men and other marginalised communities, addressing stigma, trauma, and isolation is as important as rehydration and nutrition. Practical, trauma‑informed peer support reduces shame, improves safety, and speeds recovery.
General Aftercare Routine (Body)
- Cleanse: Shower + fresh sheets.
- Oral Care: Brush teeth, rinse mouth (Biotene is good for dry mouth), and moisturise lips.
- Nourish: Drink a salty broth or electrolyte drink. Eat something soft (yoghurt/oats).
- Disconnect: Put your phone on “Do Not Disturb” for at least 4 hours.
- Connect: Send a safety text to a trusted friend: “I’m home. Just resting.”
Safety and Risks (Important)
- Hyponatremia Risk: After MDMA use, drinking excessive plain water without sodium can cause dangerously low blood sodium. Make sure to include sodium-containing fluids or salty foods at the start of recovery.
- Medication Interactions: Grapefruit can interact with many drugs; avoid it if you take daily medications until you have checked with a clinician for specific interactions.
- When to Get Emergency Help: Seek urgent care if you experience confusion, seizures, fainting, severe headache, chest pain, severe vomiting, or signs of overheating.
- If you live in the UK, call 999 or 112 if you experience any of these.
- The suicide and crisis hotline in the U.S. and Canada is 988/911.
Recovery and Self‑Care is Strength, Not Shame
In the hours after chemsex, it’s easy to slip into shame and self‑blame or feel like punishing yourself. But self‑care, listening to your body, and asking for help when needed are not signs of weakness—they are acts of self‑respect and strength. They show that you recognise your needs, honour your limits, and choose recovery over punishment.
The way you treat yourself in the hours and days after chemsex shapes your health, your mood, and your ability to make grounded choices going forward.
For Black gay men, self‑care also means stepping away from the cultural expectations around masculinity and choosing your body over the performance of hardness and silence. Refusing the pressure to “tough it out” is not weakness or a failure of manhood; it’s liberation.
Always Remember:
- Vulnerability—choosing to be honest about our struggles—is an act of courage.
- Resilience — the ability to “get up every time” after a setback — is a testament to true inner strength.
References
- Baggott, M. J., Garrison, K. J., Coyle, J. R., Galloway, G. P., Barnes, A. J., Huestis, M. A., & Mendelson, J. E. (2016). MDMA Impairs Response to Water Intake in Healthy Volunteers. Advances in Pharmacological Sciences, 2016, 1–11. https://doi.org/10.1155/2016/2175896
- DanceWize NSW. (n.d.). Managing comedowns. https://www.dancewizensw.org.au/managing-comedowns
- MedlinePlus. (n.d.). Low blood sodium (hyponatremia). https://medlineplus.gov/ency/article/000394.htm
- MedlinePlus. (2024). Fluid and electrolyte balance. https://medlineplus.gov/fluidandelectrolytebalance.html
- Office of Dietary Supplements, NIH. (2022). Magnesium: Fact sheet for health professionals. https://ods.od.nih.gov/factsheets/magnesium-healthprofessional/


